Previon helps healthcare organizations minimize risk and provides comprehensive support for all regulated enrollee communications.
With nearly two decades of experience designing and implementing large-scale document fulfillment programs, Previon Compliance helps increase your healthcare risk management program’s ROI without compromising quality or compliance.
Previon Compliance Helps PBMs and Payers:
Minimize risk and facilitate compliance
Improve enrollee communications

Increase productivity of teams managing your programs

Proactively meet the evolving needs of healthcare consumers
How Previon Compliance Works
Today’s pharmacy benefit management and health plan organizations know well that the consequences of not staying ahead of CMS compliance guidelines can be severe.
Our HIPAA-compliant software solution for payers, pharmacy benefit management organizations, third-party administrators and employer groups address the sometimes conflicting demands of federal and state regulations, while also working to improve their members’ experience.

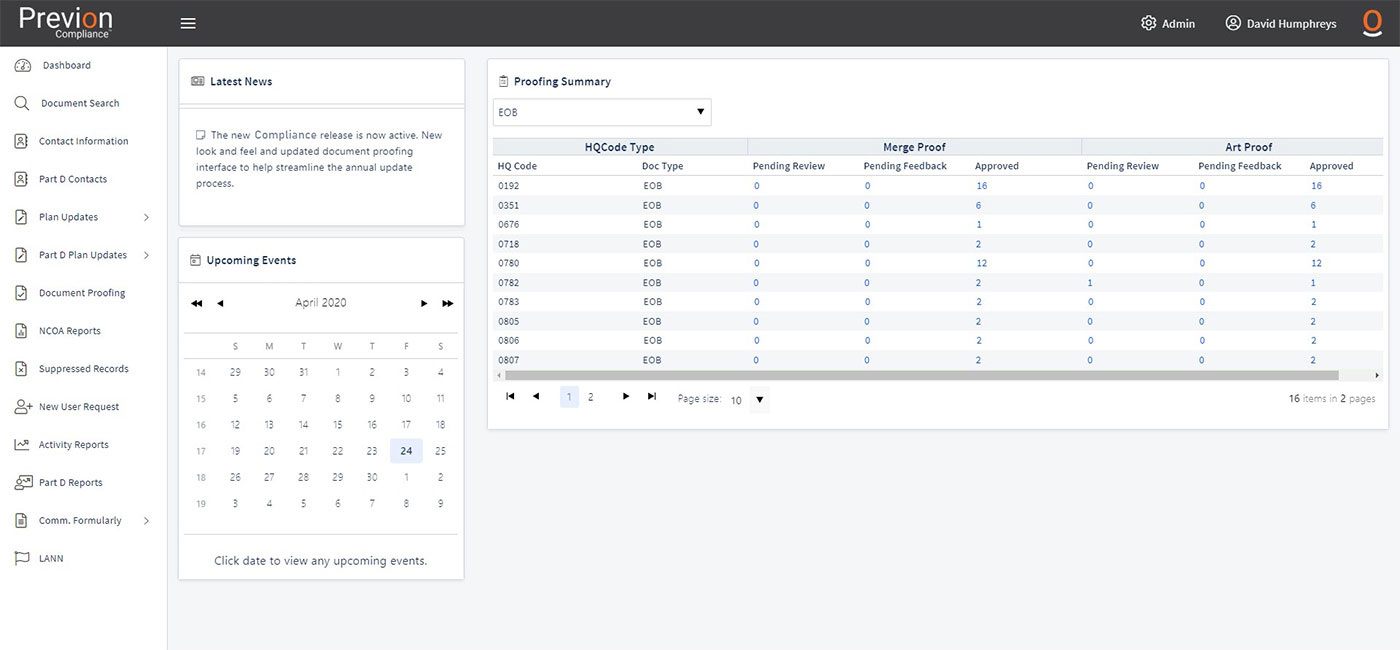
Program teams have online access to digital dashboards

Comprehensive professional service support for all aspects of regulated enrollee communications

Access, manage and update communications

Access to digital archives to support quality and audit support teams

Alternative formats like digital delivery, braille and large print

Translated language document support
Self-service updates and proofs online
Comprehensive Program Control
Healthcare professionals can manage their Compliance programs every step of the way from a simple dashboard that includes:
- Comprehensive document management
- Online editing
- Ability to approve proofs
- Sent documents archive
- Access to critical data delivery information and other program metrics